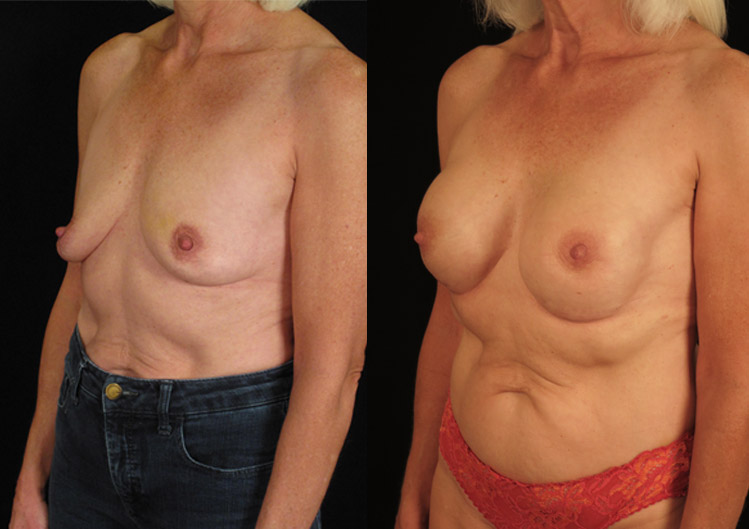
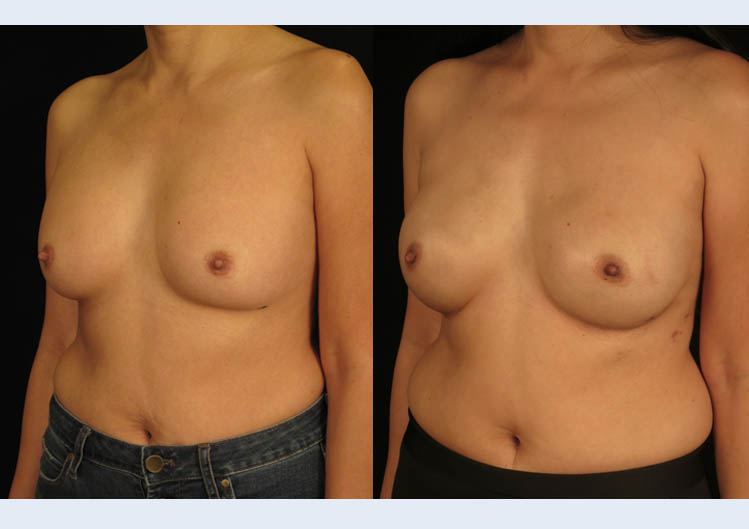
KR, Age 41
Breast Reconstruction
Patient-specific goals
A 41-year-old woman with newly diagnosed right breast cancer who decided upon a plan for a double mastectomy with removal of the nipple and areolas. Surgery was all that was necessary, she did not require chemotherapy or radiation. Her goals were to maintain a natural shape to the breast and have a similar, but slightly fuller volume.
Our Solution
We planned and performed a two-stage implant-based breast reconstruction with initial temporary expander implants placed partially below the muscle. Round silicone implants were subsequently used to create the final breast mound. At 3 months, nipple and areola reconstruction was performed to complete the creation of a natural breast shape, sized to her desire.

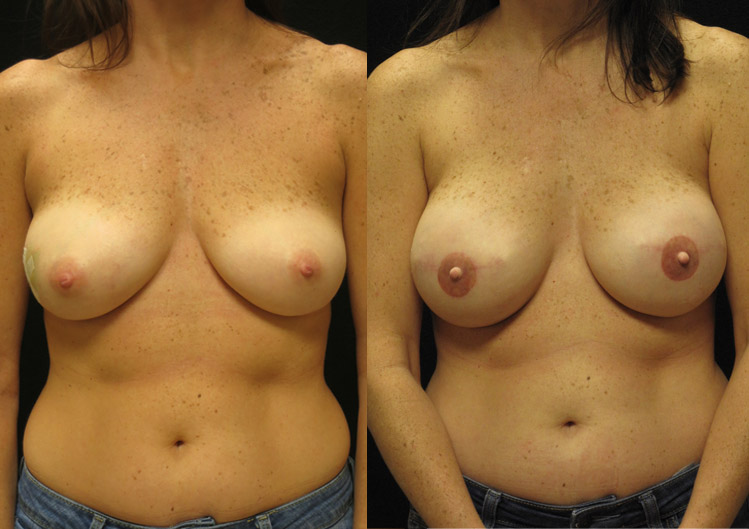








 Jennie, Age 49,
Jennie, Age 49,