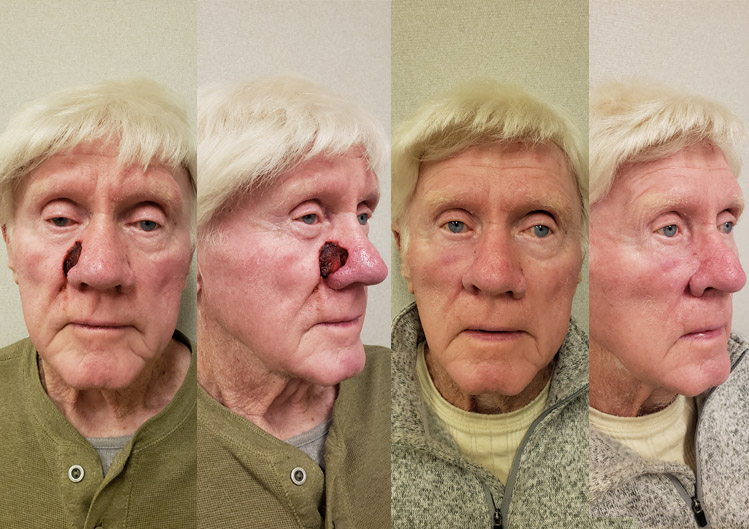
WG, Age 76
Nasal Reconstruction
Patient-specific goals
This gentleman is a 76-year-old with a complex squamous cell carcinoma of the nose. The tumor involved the full thickness of tissue of the left side of the nose. Tumor removal involved removing the left half of the nose, part of the cheek and upper lip tissues.
Our Solution
We planned and performed a three-part staged procedure starting at the tumor removal surgery with simply skin grafting the opening and stabilizing the defect. Secondarily, a forehead flap surgery allowed similar texture skin to be moved from the forehead to the nose. A final revision shaping procedure was done to get an overall nice result given the complexity of the nasal defect.